PERSISTENT Postural Perceptual Dizziness (PPPD)

PPPD is a common and well-recognised cause of chronic dizziness, that can be treated successfully. It is a form of dizziness that is not explained by damage or dysfunction to the inner ear balance organs or their brain connections i.e. the vestibular system. Structurally the vestibular system is ‘working’ or ‘functional’ but people continue to experience persistent dizziness and sense of imbalance, which can sometimes be relieved when distracted or absorbed in concentration. The persistent dizziness symptoms of PPPD then emerge as vertigo from the triggering event resolve.
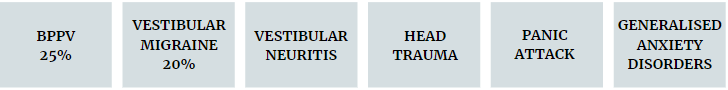
In many cases, PPPD is triggered by an acute true vestibular episode such as:
HOW DO WE DIAGNOSE PPPD?
At least one of: dizziness, unsteadiness, or non-spinning vertigo (present on most days for 3 months or more)
- Symptoms last for prolonged periods, but severity may fluctuate
- Symptoms need not be present continuously throughout the day
Persistent symptoms occur without specific provocation, but worsened by:
- Upright posture (sitting, standing, walking)
- Active or passive motion of head or body, irrespective of direction or position
- Exposure to moving visual stimuli or complex visual patterns (e.g looking at traffic passing, crowds, supermarkets)
The disorder is usually precipitated by conditions that cause acute
vestibular symptoms or difficulty with balance but may develop gradually
- When precipitated by an acute or episodic condition, symptoms settle into the pattern of criterion A with trigger resolution, but maybe intermittent before later becoming persistent
- When precipitated by a chronic syndrome, symptoms may develop slowly and worsen gradually
Symptoms cause significant distress or functional impairment such as avoiding driving, housework or movement.
Symptoms are not better accounted for by another disease or disorder
| Vestibular function tests are often normal but still are an important part of the diagnostic process, to rule out other inner ear conditions. To complicate matters, PPPD can co-occur with structural vestibular and other neurological disorders. For example, Meniere’s Disease, Vestibular Migraine and BPPV may trigger PPPD but also continue to occur episodically, resulting in acute vertigo episodes on a background of persistent dizziness. |
|
WHY DO PEOPLE DEVELOP PPPD?
Our brains use three main sources of information for balance and spatial orientation- the vestibular, somatosensory (muscle and joint senses) and visual systems. Balance responses and spatial orientation are usually automatic, subconscious and based on our past experiences. During a true vertigo episode, such as BPPV, the normal physiological reaction is for the brain to switch sensory modes to rely more on the visual and somatosensory systems; become more conscious of our balance sensations/ responses and also to adopt protective balance strategies, such as stiffening up or avoiding triggering movements to prevent falling or an increase in symptoms. Once the acute trigger has subsided, instead of reverting back to normal balance
processing and function, a maladaptive cycle can arise and result in the chronic dizziness and perceived imbalance symptoms of PPPD.
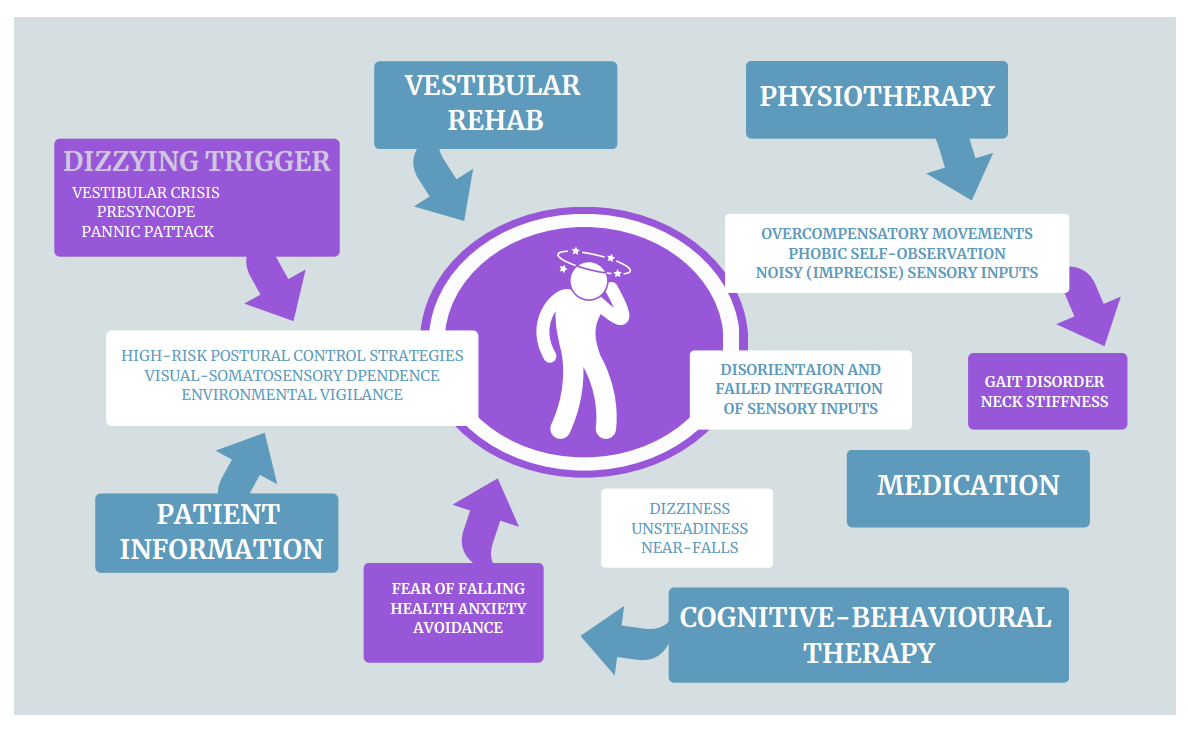
For people who go on to develop PPPD, their brains don’t switch out of ‘crisis’ mode, even though the physical cause of the vertigo trigger has resolved. The limbic system (responsible for
our fight, flight, freeze response) is thought to remain activated and the brain continues to be on ‘red alert’ to any perceived threat. The brain is hyper-vigilant with excessive self-monitoring of normal motion sensations and continues with over reliance on vision for balance.
The PPPD brain tends remain overly sensitive to slight discrepancies between anticipated and actual postural motion, again increasing hypervigilance to balance sensations, further perpetuating this unhelpful cycle. The continued use of protective balance strategies (such as walking tentatively or avoiding head movements) can produce secondary effects including muscle pain/fatigue and neck stiffness. People with PPPD can be very fearful of falling, but literature tells us they actually rarely fall.
HOW CAN PHYSIOCARE ASSIST IN MANAGING PPPD?
The aim of therapy for PPPD is to readapt the system/brain to normal function by reducing anxiety and self-monitoring, habituating to provoking factors, and promoting automatic movement control until recovery is achieved. Treatment options include:
| Vestibular and Balance Physiotherapy | Individualised specific exercises to desensitise and retrain the balance system, reduce visual dependence, manage neck stiffness/headache and other secondary effects. |
| Psychological Therapy | Cognitive behavioural therapy (CBT) to reduce hypervigilance and anxiety, and related behaviours |
| Medical Management | Certain medications can alter interactions between visuospatial, postural and emotional brain networks. A Neurologist or GP is best to advise on this option |